UCLA microbiologist Patricia J. Johnson elected to National Academy of Sciences

Patricia J. Johnson
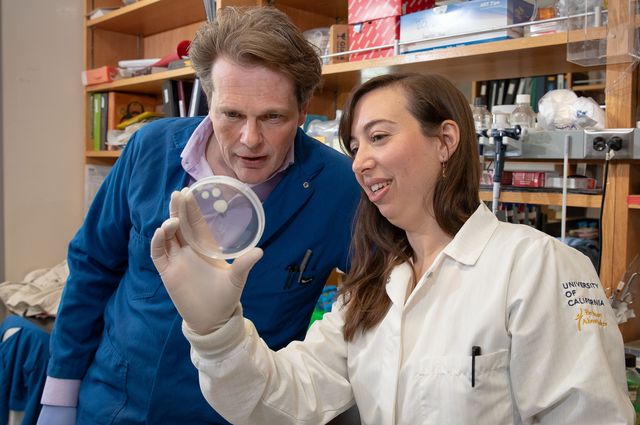
Patricia J. Johnson, UCLA professor of microbiology, immunology and molecular genetics, was elected to the National Academy of Sciences in recognition of her “distinguished and continuing achievements in original research.”
Membership in the academy is one of the highest honors that a U.S. scientist can receive. Its members have included Albert Einstein, Thomas Edison, Orville Wright and Alexander Graham Bell. The academy today announced the election of 100 new members and 25 foreign associates.
“I am very honored to be include among the ranks of such distinguished scientists,” said Johnson, who has appointments in the David Geffen School of Medicine at UCLA and the division of life sciences in the UCLA College.
Research in Johnson’s laboratory focuses on the molecular and cellular biology of a single cellular parasite called Trichomonas vaginalis. This microbe is responsible for the most prevalent, non-viral, sexually transmitted infection worldwide and is the most common parasite found in the U.S. population. An estimated 275 million people worldwide have the parasite, including approximately 3.7 million in the United States. In 2014, the Centers for Disease Control and Prevention identified trichomoniasis, the infection caused by T. vaginalis, as one of the “neglected parasitic infections in the United States.”
Johnson said that beyond its medical importance, T. vaginalis is a fascinating organism for conducting research on the evolution of biological processes present in all eukaryotes, from microbes to humans. The parasite’s atypical properties offer possible chemotherapeutic targets and vaccine candidates, she said.
Her laboratory focuses on several aspects of trichomonad biology, including its evolution, regulation of gene expression, drug resistance, genomics and biological processes vital for human infection.
“Our interdisciplinary research program merges several specialties, including structural and cell biology, biochemistry, genomics, proteomics, bioinformatics, evolution and medical sciences,” she said. “In recent years, we have narrowed our focus to defining and explaining critical pathogenic mechanisms that allow T. vaginalis to establish and maintain an infection. These studies include identifying critical parasite cell surface molecules and secreted vesicles, as well as defining human immune responses to parasitic infection. We have also investigated a possible link between infection with T. vaginalis and prostate cancer.”
The National Academy of Sciences was established in 1863 by a congressional act of incorporation signed by Abraham Lincoln that calls on the academy to act as an official adviser to the federal government, upon request, in any matter of science or technology. The academy is a private organization of scientists and engineers dedicated to the furtherance of science and its use for the general welfare.